Parkinson’s patients experienced 2.5 times better symptom improvement when doctors targeted a specific brain network rather than adjacent areas. This breakthrough challenges decades of understanding about the neurological disorder, shifting focus from a single malfunctioning brain region to a network gone haywire. The discovery offers hope for 10 million people worldwide living with Parkinson’s—and it’s already showing clinical results that could transform treatment approaches.
The SCAN Network Changes Everything
Researchers identified hyperconnected brain wiring as the root cause of movement and cognitive symptoms.
An international team analyzed brain scans from 863 participants across research centers in the US and China, publishing results in Nature this February. They identified the somato-cognitive action network (SCAN)—think of it as mission control for translating thought into movement—as hyperconnected to deep brain structures in Parkinson’s patients.
This overactive wiring disrupts everything from walking to emotional regulation, explaining why Parkinson’s affects far more than just movement. The pattern appeared only in Parkinson’s patients, not those with other neurological conditions like essential tremor or dystonia.
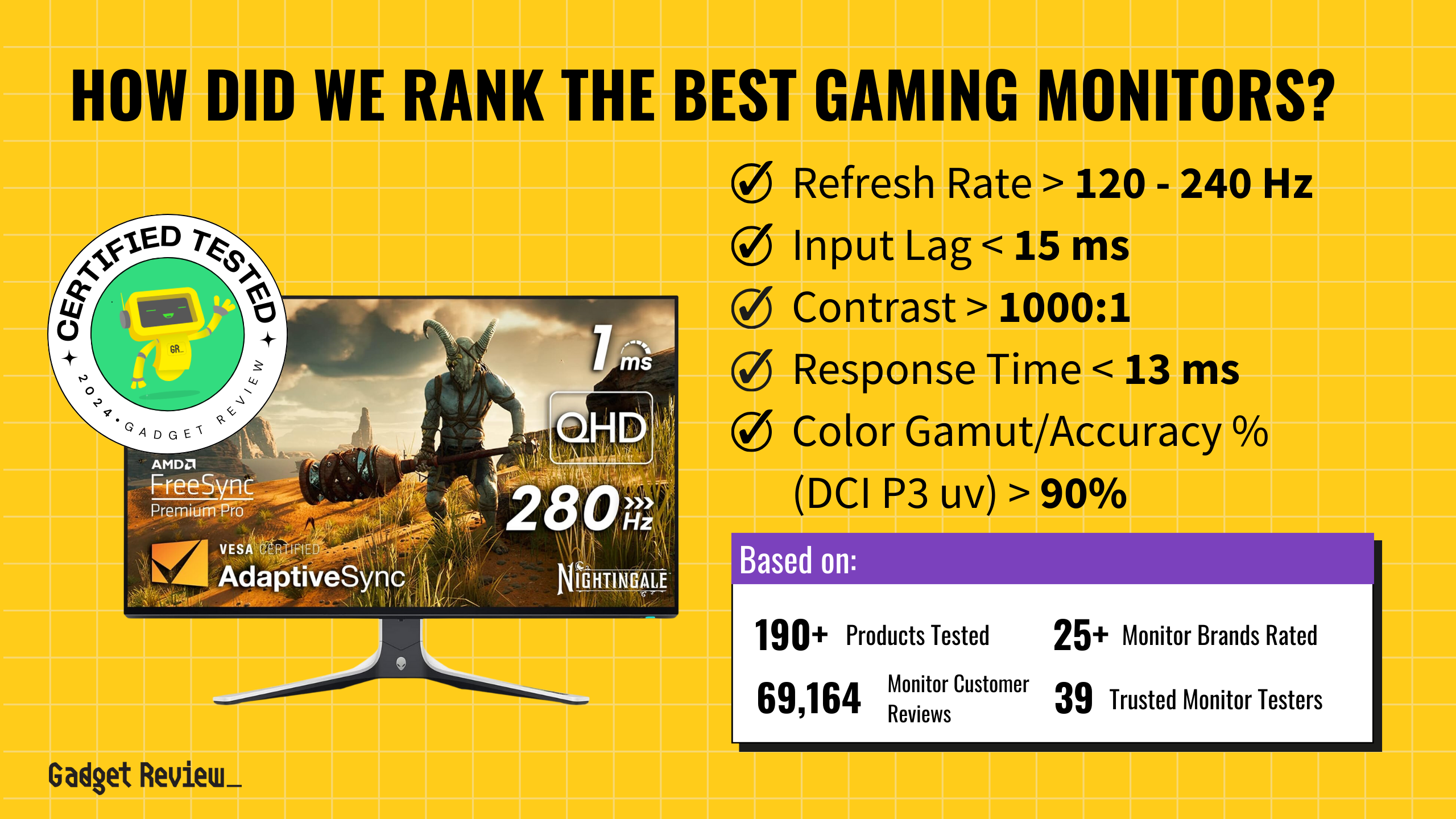
Non-Invasive Treatment Shows Major Promise
Magnetic brain stimulation targeting SCAN achieved 56% response rates versus 22% for standard approaches.
In a precision transcranial magnetic stimulation trial, 18 patients received SCAN-targeted therapy while 18 got stimulation to nearby brain regions. The SCAN-targeted group saw significant motor improvements after just one week, with 56% achieving meaningful symptom relief compared to the control group’s 22% response rate.
“With non-invasive treatments, we could start treating with neuromodulation much earlier than is currently done with DBS because they don’t require brain surgery,” explained Dr. Nico Dosenbach, who co-founded startup Turing Medical to commercialize the approach.
From Movement Disorder to Network Disease
The discovery reframes Parkinson’s as a systems-level dysfunction affecting multiple brain functions.
Senior researcher Dr. Hesheng Liu emphasized that “the disease is rooted in a much broader network dysfunction” than previously understood. The SCAN network connects to all major deep brain stimulation targets, suggesting current surgical approaches inadvertently work by modulating this circuit.
This explains why Parkinson’s involves depression, cognitive decline, and digestive issues alongside tremors—it’s not just a movement disorder but a coordination breakdown between action planning and execution.
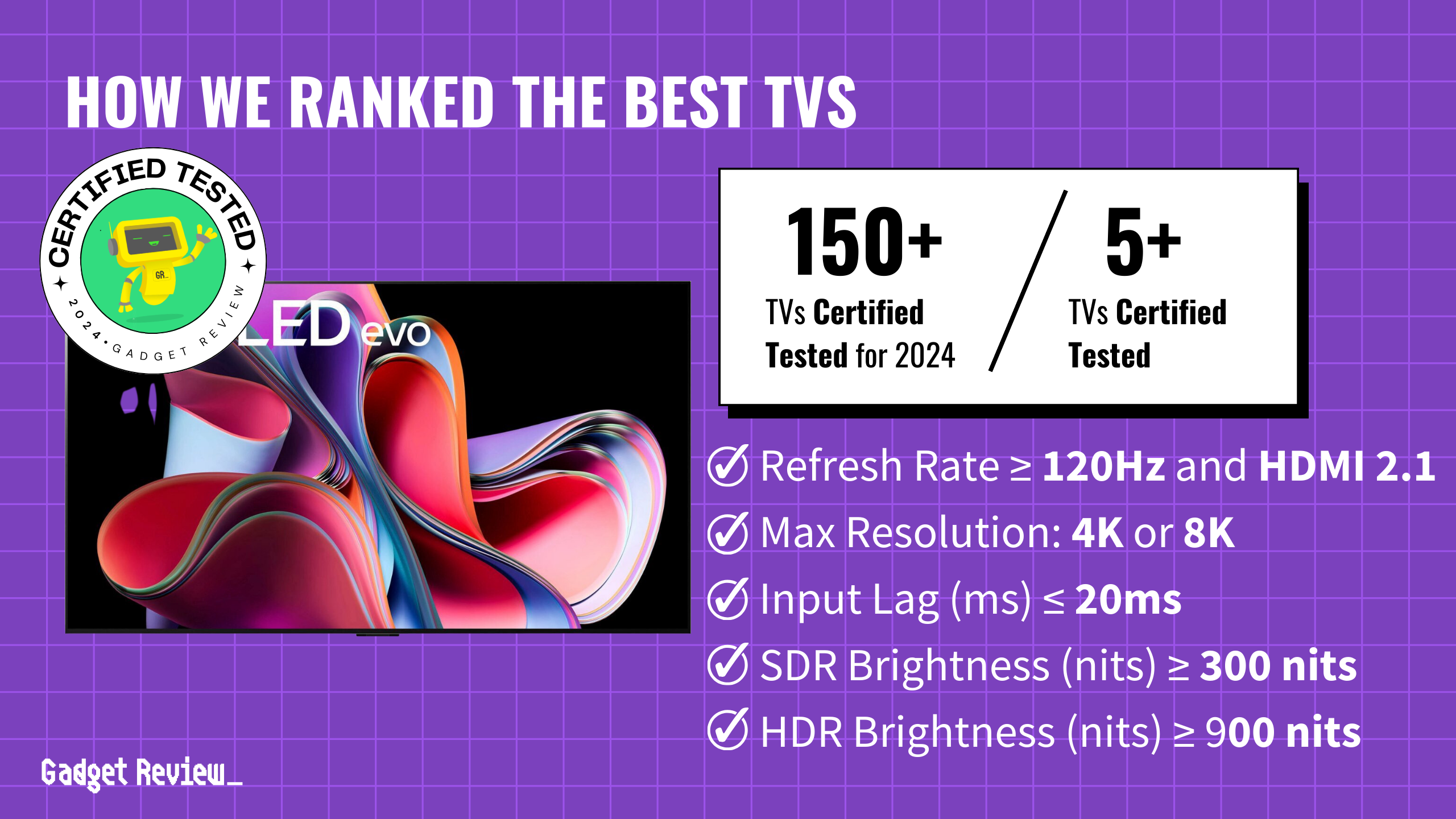
Clinical Trials Target Gait Freezing
Surface electrode strips could offer early intervention without invasive surgery.
While promising, researchers acknowledge the need for larger trials beyond their 36-person study. Turing Medical plans clinical trials using surface electrode strips placed over SCAN regions to address gait freezing—those terrifying moments when Parkinson’s patients suddenly can’t move their feet.
If validated, this precision approach could enable treatment years before symptoms become severe enough to warrant brain surgery, potentially slowing disease progression rather than just managing symptoms.